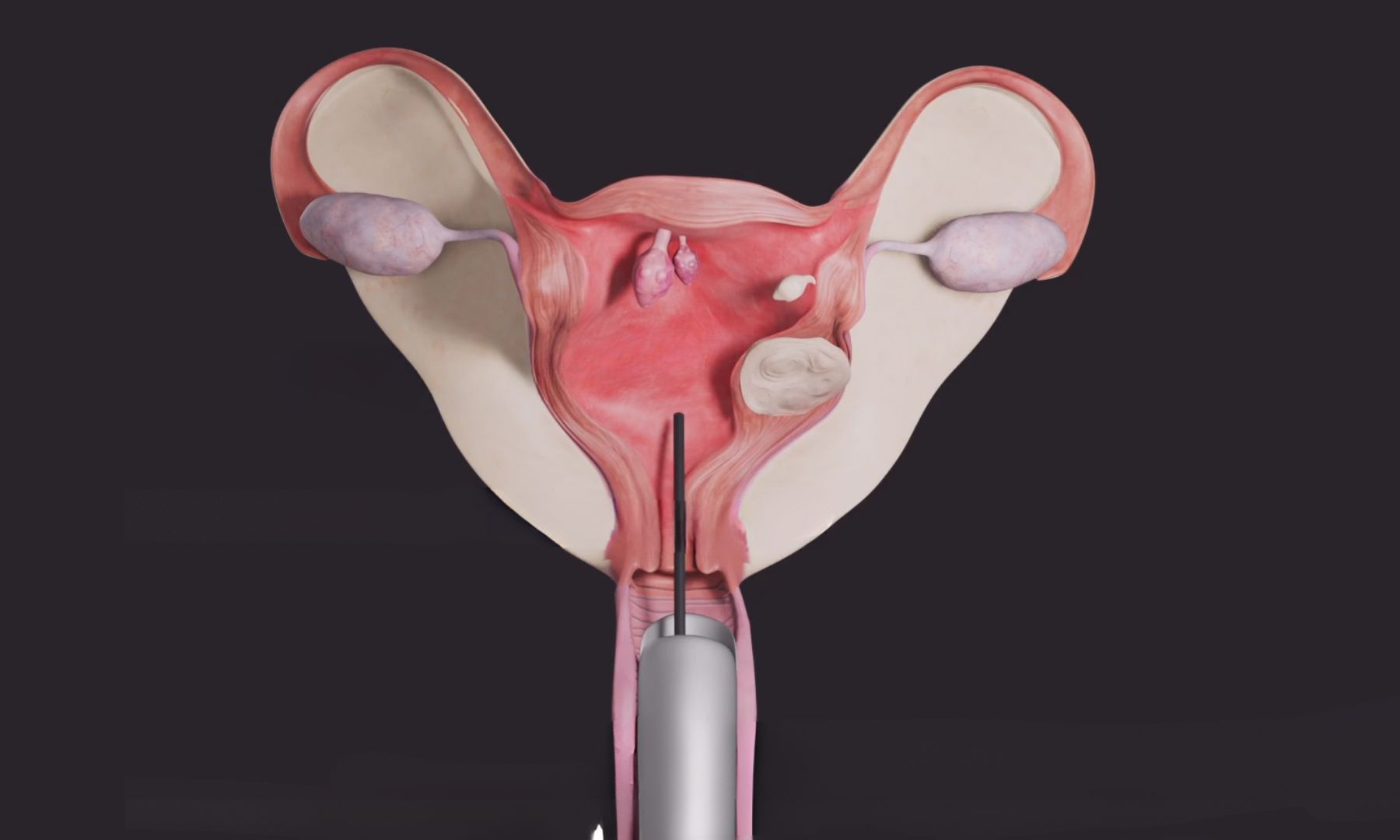
Hysteroscopy is a minimally invasive surgical procedure that allows doctors to examine the inside of the uterus using a thin, lighted instrument called a hysteroscope. The hysteroscope is inserted through the vagina and cervix into the uterus, providing a direct view of the uterine cavity.
Here are some key points about hysteroscopy:
Diagnostic Hysteroscopy:
- Purpose: Diagnostic hysteroscopy is performed to investigate and diagnose various uterine conditions or abnormalities that may be causing symptoms or fertility issues.
- Procedure: A hysteroscope is inserted into the uterus, and carbon dioxide gas or a liquid solution is used to expand the uterine cavity, allowing for better visualization. The doctor can examine the uterine lining, identify abnormalities, and possibly take tissue samples (biopsies) for further analysis.
- Indications: Diagnostic hysteroscopy may be recommended for investigating conditions such as abnormal uterine bleeding, recurrent miscarriages, unexplained infertility, suspected uterine abnormalities (e.g., fibroids, polyps, adhesions), or to evaluate the uterine cavity before certain fertility treatments.
Operative Hysteroscopy:
- Purpose: Operative hysteroscopy involves not only diagnosis but also the treatment of certain uterine conditions during the same procedure.
- Procedure: After the diagnostic evaluation, additional instruments are used through the hysteroscope to perform various surgical procedures. These may include removing polyps or fibroids, resecting adhesions, removing uterine septum (a congenital abnormality), or treating other uterine abnormalities.
- Advantages: Operative hysteroscopy is a minimally invasive approach that can often be performed on an outpatient basis, avoiding the need for a large abdominal incision. Recovery time is typically shorter compared to open surgery.
Possible Risks and Complications:
- Infection: Although rare, there is a small risk of infection following hysteroscopy.
- Uterine Perforation: In rare cases, the hysteroscope may accidentally puncture the uterine wall, which may require further intervention or surgery.
- Fluid Overload: If fluid is used to expand the uterus during the procedure, there is a slight risk of fluid overload, which can be managed by monitoring fluid absorption.
- Bleeding: Some minor bleeding may occur after hysteroscopy, but it usually resolves on its own.
Recovery and Follow-up:
- Recovery: Recovery time after hysteroscopy is generally short. Patients may experience mild cramping or spotting for a few days. Most women can resume normal activities within a day or two.
- Follow-up: Depending on the findings and procedures performed, follow-up visits may be necessary to monitor progress or address any further treatment needs.
Hysteroscopy is a valuable tool for diagnosing and treating various uterine conditions. It is important to discuss the procedure, potential risks, benefits, and expected outcomes with a healthcare provider specializing in gynecology or reproductive medicine to determine the most appropriate course of action for individual circumstances.